Safety in mind as Prescient Therapeutics develops next-generation CAR-T platform
Tragedy struck the CAR-T space this month with a US company halting a trial of its lead therapy after the deaths of two patients, a sobering reminder of the dangers involved in cell therapy. Image: Getty
Tragedy struck the CAR-T space this month with a US company halting a trial of its lead therapy after the deaths of two patients, a sobering reminder of the dangers involved in cell therapy.
The patients reportedly died from immune effector cell-associated neurotoxicity syndrome (ICANS). During CAR-T treatment, a patient’s white blood cells are engineered to fight cancer, but in these cases they attacked healthy cells.
Prescient Therapeutics (ASX:PTX) is developing a next-generation CAR-T platform called OmniCAR, based on technology licensed from the University of Pennsylvania, a pioneer in the space, as well as Oxford University.
Chief executive Steven Yatomi-Clarke acknowledges that some industry observers had assumed that safety was no longer a serious issue for CAR-T, but this latest tragedy puts safety back into sharp focus. Prescient’s OmniCAR platform seeks to make CAR-T therapy safer by enabling clinicians to control its activity even once infused into a patients
Right now, CAR-T involves injecting living cells into a patient’s body – their own genetically modified blood.
“Once these current generation CAR-T cells are infused, they propagate of their own accord, and you’ve got no way of controlling it,” Yatomi-Clarke says.
“If a doctor gives you any other medication, if you have a bad reaction, what do they tell you to do? To stop taking it, reduce the dose, or maybe change medications. But when the medicine is a living cell you can’t yet do that.”
‘Druggable and controllable’
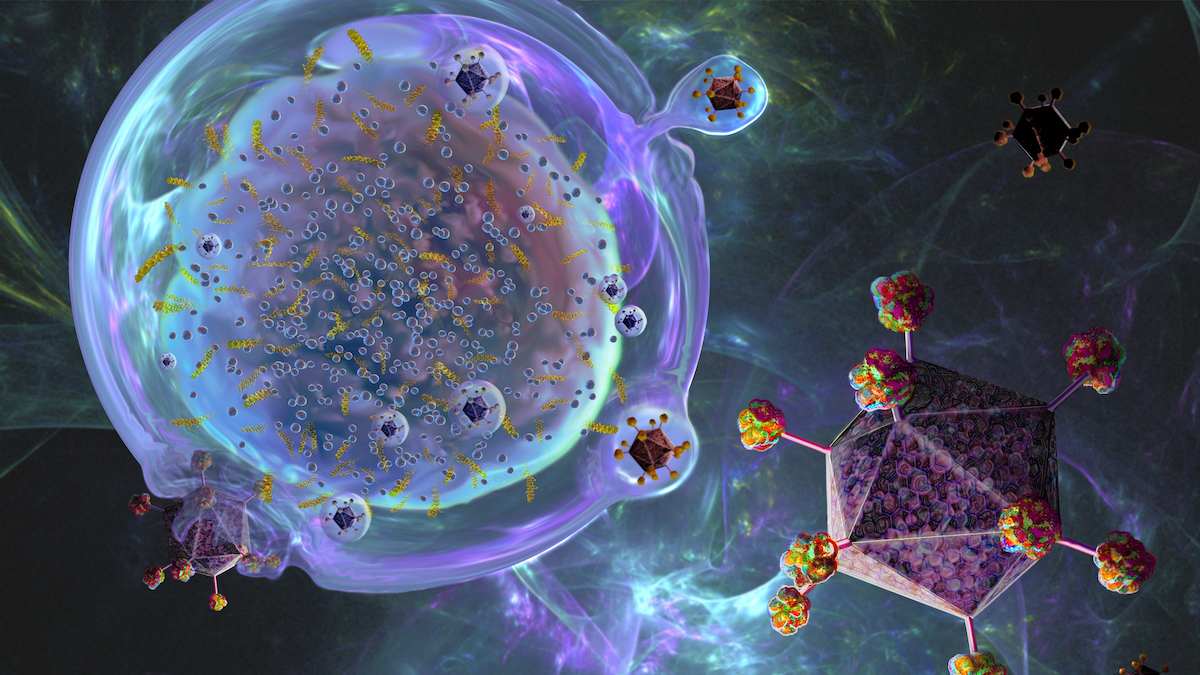
But OmniCAR is different from current generation CAR-Ts. It is designed to be controlled even after it is infused into the patients. The key to this is the modular nature of the platform, which separates the CAR-T cell and the part that binds to the cancer cells. The therapy is viable but inactive until the two components come together and bind the cancer cells.
“We’re making CAR-T cells druggable and controllable,” Yatomi-Clarke says. “Basically we are combing all of the good things about a T-cell – it can kill a cancer cell like nothing else – but giving it the control and flexibility that a doctor typically expects from a traditional medicine.”
Yatomi-Clarke says traditional CAR-T therapies are like sending soldiers into battle with a single weapon, a single map, and no communication and control in the field.
“Whereas what we’ve got is a soldier, because of this modularity, we can arm it with any weapon, send it anywhere, direct it against any target, and have full communication and control.”
The activity of the OmniCAR cells can be increased or decreased to achieve safe and efficacious levels. And even if the patient has a deleterious effect, a physician could simply stop administering the binder, and the engineered white blood cells would switch off.
“Because you can control it, it’s not a runaway train,” Yatomi-Clarke says.
The doctor could later try the therapy again at a lower dose, without the need to manufacture and administer new CAR-T cells, he said.
This plug-and-play approach is also useful if the cancer mutates, which is a problem facing current generation CAR-T. Currently in that case the patient would be left with “all of the bad side effects of CAR-T, and zero benefits, Yatomi-Clarke says. But with OmniCAR the physician could simply switch out the binder, and the T-cells would be redirected to the new target.
As Stockhead reported on Thursday, Prescient confirmed that manufacturing is complete for a range of binders that target multiple cancers.
The eventual goal is to have off-the-shelf cell therapies, so doctors don’t have to spend 22 days harvesting and manufacturing a patient’s cells so they can be infused into their body, Yatomi-Clarke says.
Please find link to PTX’s webcast on Thursday, 1 July here.
This article was developed in collaboration with Prescient Therapeutics, a Stockhead advertiser at the time of publishing.
This article does not constitute financial product advice. You should consider obtaining independent advice before making any financial decisions.
Related Topics

UNLOCK INSIGHTS
Discover the untold stories of emerging ASX stocks.
Daily news and expert analysis, it's free to subscribe.
By proceeding, you confirm you understand that we handle personal information in accordance with our Privacy Policy.